Life as a Hospice & Palliative Care NP
Find NP Schools
For the latest academic year, we have over 180 NP schools in our database and those that advertise with us are labeled “sponsor”. When you click on a sponsoring school or program, or fill out a form to request information from a sponsoring school, we may earn a commission. View our advertising disclosure for more details.
“We have a real need for providers who are skilled and educated in hospice and palliative care. Policy-wise, we could do more to incentivize NPs to enter this field.”
Karen Hyden, PhD, CSU Shiley Haynes Institute for Palliative Care
Palliative care is a medical specialty focused on improving the quality of life for patients facing serious illnesses and the side effects of their treatment; hospice care focuses on the palliation of terminally ill patients toward the end of their life. Both are of critical importance.
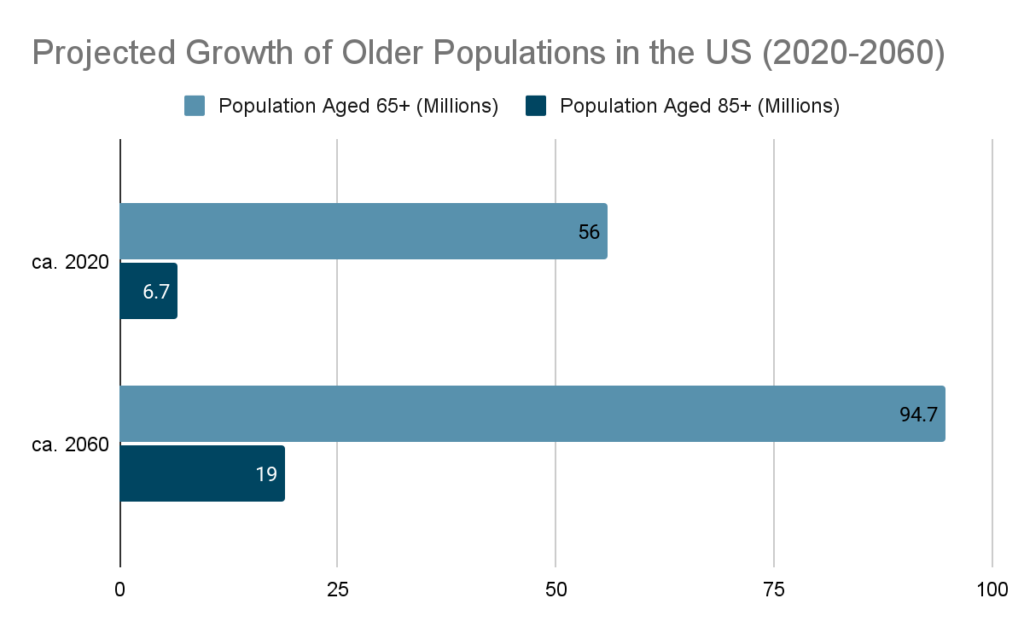
Approximately 90 million Americans live with a serious illness (JAMA), and that number is expected to more than double over the next 25 years as the Baby Boomers age through retirement and into old age. Adults 65 and older are projected to represent approximately 23 percent of the overall United States population by 2060 (PRB 2024).
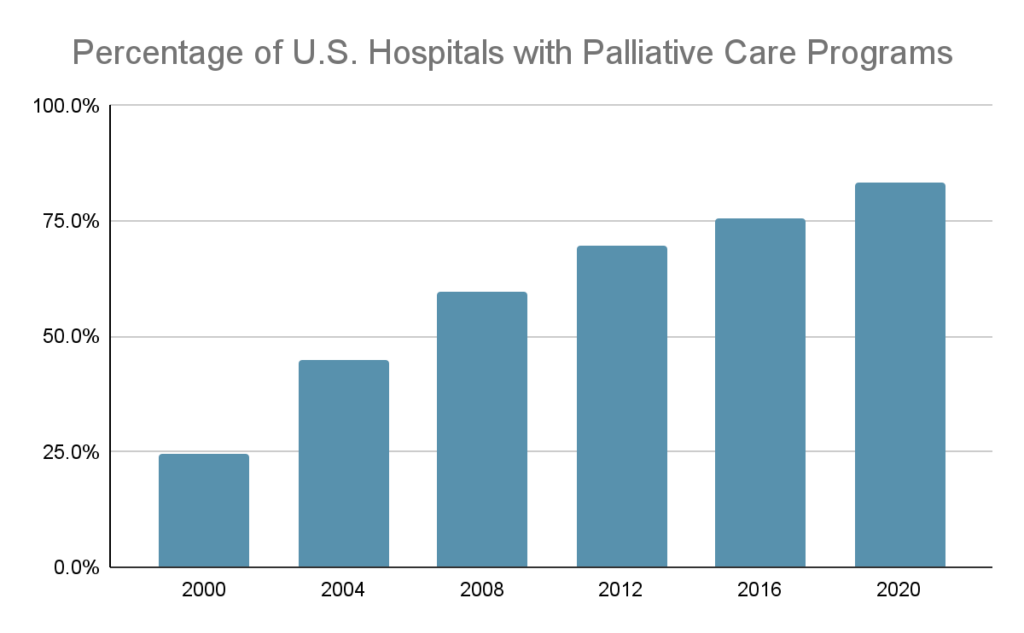
It’s not just the Baby Boomers driving demand for more palliative care, either: according to the Centers for Medicare & Medicaid Services (CMS), between 19 and 50 percent of non-elderly people have a preexisting health conditions, including life-limiting and chronic illness (CMS 2024). The percentage of hospitals (with 50 or more beds) with a palliative care program has more than tripled between 2000 and 2022, and more than 83 percent of these hospitals now have a palliative care team (CAPC 2022). Continued growth in this area calls for an influx of new palliative care professionals.
The holistic, patient-centered approach of nurse practitioners (NPs) makes them ideally suited for hospice and palliative care (Can Oncol Nurs J. 2019). In treating patients, NPs incorporate a wide range of therapies to address common symptoms like pain, nausea, anxiety, and depression.
Palliative and hospice care, as specialties, allow NPs a great deal of scope and autonomy, especially in states where they are allowed to prescribe and work more independently. And many NPs who choose to specialize in palliative and hospice care find it aligns with the reasons they got into healthcare in the first place: to deliver care in a patient-centered, whole-person environment that focuses on comfort and quality of life.
Read on to learn more about the work, advocacy, and future of hospice and palliative care NPs.
Meet the Experts

Constance Dahlin, MSN, ANP-BC, ACHPN, FPCN, FAAN
Constance Dahlin is a palliative care consultant, educator, and palliative nurse practitioner. She is a consultant to the Center to Advance Palliative Care (CAPC) in community-based care and education, and co-director of the Palliative Care APRN Externship.
Dahlin is co-editor of the Oxford University Press Advanced Practice Palliative Nursing and edited the second and third editions of the National Consensus Project’s Clinical Practice Guidelines for Palliative Care. She authored the 2021 Palliative Nursing: Scope and Standards of Practice, Competencies for the Palliative and Hospice APRN, and the Competencies for the Palliative and Hospice RN, as well as the 2017 Hospice and Palliative APRN Professional Practice Guide.
Dahlin was one of 30 individuals named as a Visionary in Hospice and Palliative Medicine by the American Academy of Hospice and Palliative Medicine (AAHPM) for their 30th Anniversary in 2018. She is a fellow of the American Academy of Nursing and a fellow of Hospice and Palliative Nursing.
Dahlin was interviewed for this feature in October 2021.

Cammie Rausch, DNP, AGPCNP-BC, ACHPN
Dr. Cammie Rausch is a nurse practitioner at the Rocky Mountain Regional VA in Denver, CO. She currently serves chronically ill veterans in their home through a program called Home Based Primary Care. She is also an instructor at the California State University Shiley Haynes Institute for Palliative Care.
Dr. Rausch received her BSN from Washington State University, and both her MSN and DNP from the University of South Alabama with a subspecialty in palliative care. She has 20 years of experience practicing in nursing, with 17 years of hospice and palliative care experience.
Dr. Rausch was interviewed for this feature in October 2021.

Karen Hyden, PhD, MSN, MEd, APN-BC, ACHPN
Dr. Karen Hyden is a distinguished nurse leader who holds a Pastoral Counseling License and is a double board-certified nurse practitioner in women’s health and hospice & palliative care. She combines her unique clinical expertise and leadership skills with a passion for creating successful care models for vulnerable populations by leading palliative care programs nationwide.
Dr. Hyden has served on the Hospice and Palliative Credentialing Board and serves on Tennessee’s Palliative Care & Quality of Life Advisory Council. An accomplished author and educator, she has contributed to evidence-based literature, including the Oxford Textbook of Palliative Nursing and has taught at the CSU Shiley Haynes Institute for Palliative Care for nearly a decade.
Dr. Hyden was interviewed for an update to this feature in 2025.
The Role of Hospice & Palliative Care NPs
Palliative care can take place in both inpatient and outpatient settings. In inpatient settings, palliative care NPs generally work as part of a collaborative team that can include physicians, nurses, social workers, and spiritual care advisors. This team assists patients who are often at a crossroads in their illness journey, and helps them set goals and secure treatments that meet those goals.
“When a patient is diagnosed with cancer, they might be given radiation and chemotherapy, which can have serious side effects like fatigue, nausea, pain, and decreased appetite,” Dr. Rausch says. “While an oncologist is adept at treating the cancer, they’re not always as focused on treating the symptoms. In a perfect world, that patient should also get a referral to a palliative care specialist to help manage those symptoms, so they could have a better quality of life. If your symptoms are managed better, you’re able to heal better. That’s palliative care.”
While patient encounters in inpatient palliative care may be episodic and brief, outpatient palliative care (which can include hospice care) is very hands-on, and often occurs over a longer period of time. Especially in community-based settings, palliative care teams can be led by hospice and palliative care NPs who work with social workers and other clinicians as needed.
“Just by our training as NPs, I feel that we are very well-suited for this specialty,” Dr. Rausch says. “Palliative care and hospice care are still not widely available or widely known about, but NPs can really help broaden the field and be good patient advocates for greater accessibility.”
The Value of Hospice & Palliative Care NPs
Both palliative care and hospice care have been shown to improve patient outcomes. A 2019 meta-analysis of randomized controlled trials found that patients with advanced cancer who received outpatient palliative care lived longer and had a better quality of life than similar patients who did not receive such care. And the use of hospice care during the last six months of life has been associated with improved patient experience, including satisfaction and pain control, as well as clinical outcomes of care, such as decreased ICU usage and lower hospital mortality.
“A lot of people think that hospice means we hook the patient up to morphine, and then sit around and sing kumbaya,” Dr. Rausch says. “And that’s just not really it. Hospice is more about aggressive symptom management at the end of life, to have a better quality of life. It’s holistic in that we care for the patient and everything around them.”
Palliative care most commonly deals with patients who have illnesses such as cancer, heart disease, Alzheimer’s, Parkinson’s, and diabetes. But it may be appropriate at any age, and at any stage in a serious illness. Often, palliative care, and especially hospice care, can involve some difficult decisions and challenging conversations. Hospice and palliative care NPs are well-suited for this: nursing has been ranked as the most trusted profession in America for 23 years in a row, and NPs who specialize in this field are experts in guiding patients to the goals and decisions that are best for them.
“It really can be a lot of fun, stepping into a relationship with a patient and family that you don’t know,” Dahlin says. “You’re stepping into the middle of a play, and all this stuff is happening. You have to figure out the cast of characters, their roles, and frameworks. You start to color stuff in and determine how the pieces come together according to what they want, and not what we as NPs may want for them.”
Advocacy Issues for Hospice & Palliative Care NPs
One of the top advocacy issues for hospice and palliative care NPs is increasing awareness of and access to hospice and palliative care. A 2015 report by the Kaiser Family Foundation found that 90 percent of adults believe that healthcare providers should discuss end-of-life issues with their patients, but only 17 percent of adults say they’ve had such conversations. Hospice and palliative care NPs are pushing to remove the fear from such discussions and push them into normalcy.
“We need more palliative care NPs who work in the hospital and work in the community,” Dahlin says. “By having palliative care NPs in geriatric clinics, in pediatric clinics, and in heart failure clinics, patients can start to see palliative care as a natural extension of traditional care.”
Access to hospice and palliative care is an even more severe issue in marginalized communities. Marginalized communities include patients who are Black, Indigenous, and people of color, but they also include patients with serious mental illnesses, dual diagnoses, substance abuse disorders, and other complicating factors.
“There are a lot of people whose experience with healthcare has not engendered trust, and those are the people who get diagnosed late,” Dahlin says. “But then how do we still help them foster their own goals, with their own way of integrity? It’s a challenge because some of the resources still aren’t there.”
The Future of Hospice & Palliative Care NPs
As the Baby Boomer generation ages, there will be an even greater need for hospice and palliative care NPs. While Baby Boomers have a longer life expectancy than previous generations, they also have higher rates of chronic disease and lower self-rated health than past generations.
“There’s definitely a shortage of palliative care and hospice providers,” Dr. Rausch says. “But Baby Boomers are more educated in terms of what’s available to them for healthcare. They’re savvier and they know that there are different options. They ask tough questions and push the envelope. I think that’s good for hospice and palliative care.”
In 2021, the American Association of Colleges of Nursing (AACN) released the latest version of its core competencies for professional nursing education. The new core competencies are split into four spheres of care, and one of those spheres is hospice and palliative care. As a result, graduate-level NP preparation programs are now mandated to include content on hospice and palliative care.
“There is truly a fine art to end-of-life care and palliative care,” Dr. Rausch says. “I think that people are starting to see that those who are dying deserve more than just hand-holding and that there is a real science to it. There’s a lot more research that’s shining a light on our field, and that’s exciting to me.”
Update 2026: Growing Awareness, Growing Impact
Over the last few years, there’s been a growing awareness of what palliative care and hospice care are and what they can offer. There’s also been a change in perception around which populations can benefit from palliative and hospice care. It’s no longer associated so heavily with oncology patients.
“Across the board, people are more aware of what hospice and palliative care can offer to patients in all disease processes,” Dr. Hyden says.
That increase in awareness around palliative and hospice extends beyond the patient to the provider and institutional level. There’s more training available for hospice and palliative care NPs than ever before. The result is a virtuous cycle, where the role of the hospice and palliative care NP is continuing to evolve and expand.
“When I started out my career in hospice, I was doing visits where I primarily just reassessed whether patients were still appropriate for the service,” Dr. Hyden says. “I wasn’t necessarily providing medical care or symptom management. But palliative care allows for NPs to be implemented into the care team, and often leading the care team.”
Where and how palliative care is provided is changing, too. Today’s palliative care providers might be embedded in oncology practices or even primary care practices. But the biggest change has been the integration of telehealth. Palliative and hospice NPs are able to take a hybrid approach, mixing remote and community visits, maintaining the human element while also extending their reach.
“Telehealth has allowed NPs to have a better quality of life and a better work-life balance without sacrificing the value of the care provided for patients,” Dr. Hyden says. “NPs are able to increase productivity by having better access to patients without introducing a lot of windshield time. It’s not appropriate for every type of patient visit, but when it is appropriate, it is a great alternative for palliative NPs.”
There’s still room to improve. Dr. Hyden would like to see more research around concurrent care, which is where hospice and palliative patients still pursue potentially life-prolonging or curative treatments. As part of an integrated, holistic approach, it opens a wider band of possibilities. It also gives patients and families peace of mind. Too often, palliative care is viewed as a bridge to hospice—but it doesn’t have to be.
“Concurrent care allows patients to get the extra support they need, resulting in having a better quality of life,” Dr. Hyden says. “We see it a lot in pediatric palliative and hospice research, and I’d love to see more research focused on concurrent care for adults.”
Today’s NPs can play a significant role in breaking palliative care out of its siloes and embedding it in different practices. That would help solve one of the specialty’s largest pain points: palliative care NPs often don’t get to work with patients long enough to build rapport and add value. When patients are admitted to palliative care too late, they end up moving to hospice relatively quickly.
“The best case scenario would be to have components of palliative care, if not a full palliative care program, embedded into more care models, and this can be done by equipping NPs with palliative care knowledge and skills,” Dr. Hyden says.
The future for hospice and palliative care NPs is bright. Further advancements in technology, and telehealth specifically, can act as a force multiplier for providers. Changes to, or pivots away from, the fee-for-service model could change the math for the better on hospice and palliative care reimbursement. And, as the need for hospice and palliative care increases, a new generation of hospice and palliative care NPs will be looked to as leaders in the field.
“We have a real need for providers who are skilled and educated in hospice and palliative care,” Dr. Hyden says. “Policy-wise, we could do more to incentivize NPs to enter this field.”
Additional incentivization could be relatively simple. Currently, medical doctors get reimbursed for their schooling if they go into hospice or palliative care, but NPs do not get reimbursed for their student loans when they pursue the extra education needed to specialize in hospice or palliative care. Those loans can be debilitating to an NP just starting their career. While there are repayment schemes for NPs—such as via HRSA—they’re conditional on working in a low-income or health professional shortage area. However, with telehealth shrinking distances and making remote care easier, the map doesn’t necessarily look like it did before. Widening the criteria for student loan reimbursement for hospice and palliative care NPs is an easy way to incentivize more future leaders in this field.
“I’ve raised my hand on this issue quite a few times,” Dr. Hyden says. “I’ll keep raising my hand.”
Resources for Hospice & Palliative Care NPs
To learn more about the work and advocacy of hospice and palliative care NPs, check out some of the resources below.
- Center to Advance Palliative Care (CAPC): The nation’s leading resource in its field, CAPC is a national organization dedicated to increasing the availability of quality healthcare for people living with a serious illness. They provide healthcare professionals and organizations with the training, tools, and technical assistance necessary to effectively meet this need.
- CSU Shiley Haynes Institute for Palliative Care: The CSU Shiley Haynes Institute for Palliative Care provides online, evidence-based, practice-focused education for healthcare professionals working in palliative and serious illness care. Their APRN Palliative Care certificate course consists of nine months of comprehensive training for NPs working in (or seeking to enter) palliative care. The Institute also offers resources for nursing faculty seeking to integrate palliative care content into undergraduate and graduate-level curricula.
- Hospice & Palliative Nurses Association (HPNA): Established in 1986, HPNA is the national professional organization that represents the specialty of palliative nursing, which includes hospice and palliative nurses. They support the profession through education programs, research initiatives, and advocacy.
Background information and resources were provided by Jennifer Moore Ballentine, MA, the executive director of the CSU Shiley Haynes Institute for Palliative Care.

Matt Zbrog
WriterMatt Zbrog is a writer and researcher from Southern California, and he believes nurse practitioners (NP) are an indispensable component of America’s current and future healthcare workforce. Since 2018, he’s written extensively about the work and advocacy of NPs, with a particular focus on the rapid growth of specialization programs, residencies, fellowships, and professional organizations. As part of an ongoing series on state practice authority, he’s worked with NP leaders, educators, and advocates from across the country to elevate policy discussions that empower NPs. His articles have featured interviews with the leadership of the American Association of Nurse Practitioners (AANP), the National Association of Pediatric Nurse Practitioners (NAPNAP), and many other professional nursing associations.